Does PCOD Go Away After Pregnancy? A Clear, Complete Guide

Understanding PCOD in Simple Terms
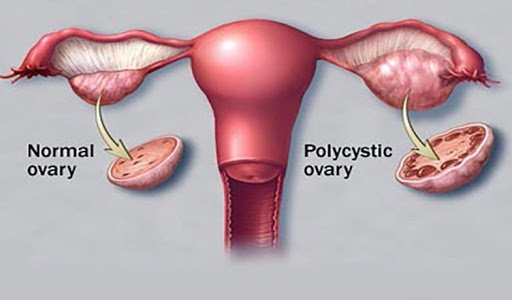
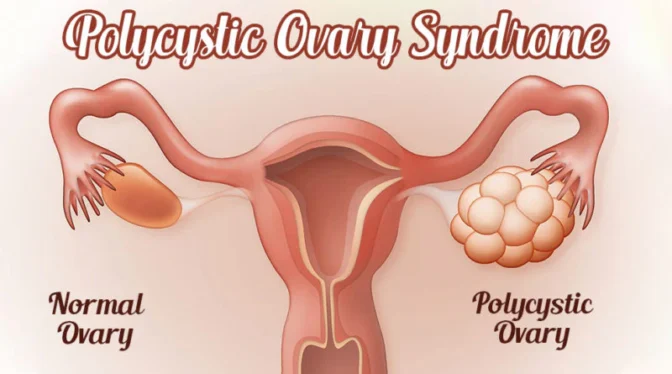
Polycystic Ovarian Disease (PCOD) is a common hormonal condition that affects women of reproductive age. It is marked by irregular ovulation, hormonal imbalance, and the presence of multiple immature follicles in the ovaries. Symptoms often include irregular periods, weight gain, acne, excess facial hair, and difficulty conceiving.
One of the most frequently asked questions we encounter is whether PCOD goes away after pregnancy. Pregnancy brings significant hormonal changes, and many women notice improvement in symptoms afterward. However, the complete picture requires a deeper understanding of how PCOD behaves before, during, and after pregnancy.
Does PCOD Go Away After Pregnancy? The Direct Answer
PCOD does not permanently go away after pregnancy, but pregnancy can significantly improve symptoms in many women. For some, menstrual cycles become more regular, ovulation improves, and hormone levels stabilize for months or even years after childbirth. For others, symptoms may return gradually once hormonal balance shifts again.
PCOD is considered a chronic metabolic and hormonal condition, not a temporary illness. Pregnancy does not cure it, but it can act as a reset phase for the body, especially when followed by healthy lifestyle changes.
Why Pregnancy Improves PCOD Symptoms
During pregnancy, the body experiences a unique hormonal environment that temporarily suppresses many PCOD-related issues.
Hormonal Stabilization

Pregnancy reduces excessive androgen production and promotes progesterone dominance. This hormonal balance often leads to:
- Regular suppression of ovarian cyst formation
- Reduced acne and hair growth
- Improved ovulatory function after delivery
Break from Irregular Ovulation
Since ovulation pauses during pregnancy, the ovaries get a functional rest. This break can improve ovarian responsiveness post-pregnancy.
Improved Insulin Sensitivity
Many women adopt healthier diets and routines during pregnancy. Better insulin regulation plays a crucial role in controlling PCOD symptoms.
PCOD After Delivery: What Usually Happens
Post-pregnancy experiences vary, but common patterns include:
- Regular periods for several months
- Reduced severity of PCOD symptoms
- Delayed return of cyst formation
- Gradual symptom recurrence if lifestyle factors are neglected
For women with mild PCOD, improvement may last long-term. For those with moderate to severe PCOD, symptoms often return without continued management.
Does Breastfeeding Affect PCOD?

Breastfeeding can help manage PCOD symptoms temporarily. Prolactin hormone levels remain high during lactation, which suppresses ovulation and reduces androgen activity.
Benefits of breastfeeding for PCOD include:
- Delayed return of irregular periods
- Improved postpartum weight loss
- Reduced insulin resistance
However, once breastfeeding stops and normal hormonal cycles resume, PCOD symptoms may reappear if not actively managed.
Can PCOD Return Years After Pregnancy?
Yes, PCOD can return years after pregnancy, especially if contributing factors persist. Common triggers include:
- Weight gain
- Sedentary lifestyle
- High sugar or refined carbohydrate intake
- Chronic stress
- Poor sleep patterns
PCOD is strongly linked to metabolic health, which means long-term symptom control depends on consistent daily habits.
Signs That PCOD Is Returning After Pregnancy
Women should watch for early signs such as:
- Increasing cycle irregularity
- Sudden weight gain around the abdomen
- Acne flare-ups
- Excessive hair fall or facial hair
- Difficulty losing postpartum weight
Early recognition allows better management without aggressive medication.
How We Can Manage PCOD After Pregnancy
While PCOD cannot be permanently cured, long-term control is absolutely achievable.
Balanced Nutrition
We recommend:
- Low-glycemic foods
- High fiber vegetables
- Lean protein sources
- Healthy fats
Avoiding sugar spikes is one of the most effective ways to control hormonal imbalance.
Consistent Physical Activity
Regular exercise improves insulin sensitivity and supports hormonal regulation. Even moderate activities like walking, yoga, or strength training offer significant benefits.
Weight Management
Maintaining a healthy weight reduces androgen production and restores ovulatory cycles in many women.
Stress Reduction
Chronic stress elevates cortisol, which worsens PCOD symptoms. Mindfulness, adequate sleep, and relaxation techniques play a critical role.
Medical Monitoring
Regular follow-ups help track hormone levels, menstrual patterns, and metabolic health. Treatment plans should always be personalized.
Can Women with PCOD Have Normal Pregnancies?
Absolutely. Most women with PCOD can conceive and carry healthy pregnancies, especially with timely diagnosis and proper care. Many women conceive naturally, while others may require minimal medical support.
Pregnancy outcomes improve significantly when PCOD is managed proactively before conception.
Myths About PCOD and Pregnancy
Pregnancy cures PCOD
Pregnancy improves symptoms but does not eliminate the condition.
PCOD always causes infertility
PCOD affects ovulation, not fertility permanently. With proper care, conception is highly achievable.
Symptoms will never return
Symptoms can return if lifestyle management is neglected.
Long-Term Outlook for Women with PCOD
PCOD is a manageable condition, not a life sentence. Women who maintain healthy routines often experience:
- Regular cycles
- Balanced hormones
- Improved energy levels
- Reduced long-term health risks
Post-pregnancy is a powerful opportunity to build habits that keep PCOD under control for life.
Final Thoughts: Does PCOD Go Away After Pregnancy?
PCOD does not permanently disappear after pregnancy, but pregnancy can significantly reduce symptoms and improve hormonal balance. The long-term outcome depends on how well the body is supported afterward. With proper nutrition, exercise, stress control, and medical guidance, many women live symptom-free for years.